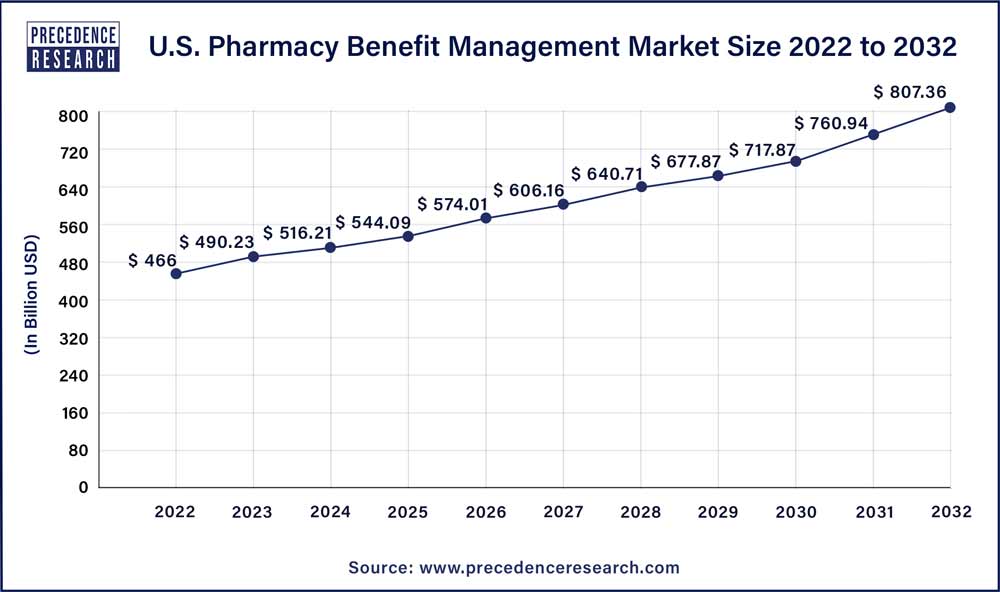
The global U.S. pharmacy benefit management market size was estimated to be around US$ 513.26 billion in 2022. It is projected to reach US$ 1,219.54 billion by 2032, indicating a CAGR of 9.04% from 2023 to 2032.
Key Takeaways:
- By Business Model, the standalone PBM segment dominated the market with the largest market share of 60% in 2022.
- By Business Model, the healthcare insurance provider segment is expected to generate significant revenue throughout the forecast period.
- By Services, the specialty pharmacies segment dominated the market in 2022.
- By Services, the retail services segment is expected to witness significant growth during the predicted timeframe.
- By End-user, the commercial segment projected the highest market growth in 2022.
- By End-user, the federal segment is expected to dominate the market during the anticipated time period.
The market research report on the U.S. pharmacy benefit management market provides a comprehensive analysis of various key aspects. It includes the definition, classification, and application of U.S. pharmacy benefit management products. The report examines the development trends, competitive landscape, and industrial chain structure within the industry. Furthermore, it presents an overview of the industry, analyzes national policies and planning, and offers insights into the latest market dynamics and opportunities at a global level.
Get a Sample: https://www.precedenceresearch.com/sample/3225
Report Scope of the U.S. Pharmacy Benefit Management Market:
| Report Coverage | Details |
| Market Size in 2023 | USD 559.66 Billion |
| Market Size by 2032 | USD 1,219.54 Billion |
| Growth Rate from 2023 to 2032 | CAGR of 9.04% |
| Base Year | 2022 |
| Forecast Period | 2023 To 2032 |
| Segments Covered | By Business Model, By Service, and By End-user |
Read More: Engineered T Cells Market Size to Garner USD 348.9 Billion by 2032
The report presents the volume and value-based market size for the base year 2022 and forecasts the market’s growth between 2023 and 2032. It estimates market numbers based on product form and application, providing size and forecast for each application segment in both global and regional markets.
Focusing on the global U.S. pharmacy benefit management market, the report highlights its status, future forecasts, growth opportunities, key market players, and key market regions such as the United States, Europe, and China. The study aims to present the development of the U.S. pharmacy benefit management market by considering factors like Year-on-Year (Y-o-Y) growth, in addition to Compound Annual Growth Rate (CAGR). This approach enables a better understanding of market certainty and the identification of lucrative opportunities.
Regarding production, the report investigates the capacity, production, value, ex-factory price, growth rate, and market share of major manufacturers, regions, and product types. On the consumption side, the report focuses on the regional consumption of U.S. pharmacy benefit management products across different countries and applications.
Buyers of the report gain access to verified market figures, including global market size in terms of revenue and volume. The report provides reliable estimations and calculations for global revenue and volume by product type from 2023 to 2032. It also includes accurate figures for production capacity and production by region during the same period.
The research includes product parameters, production processes, cost structures, and data classified by region, technology, and application. Furthermore, it conducts SWOT analysis and investment feasibility studies for new projects.
This in-depth research report offers valuable insights into the U.S. pharmacy benefit management market. It employs an objective and fair approach to analyze industry trends, supporting customer competition analysis, development planning, and investment decision-making. The project received support and assistance from technicians and marketing personnel across various links in the industry chain.
The competitive landscape section of the report provides detailed information on U.S. pharmacy benefit management market competitors. It includes company overviews, financials, revenue generation, market potential, research and development investments, new market initiatives, global presence, production sites, production capacities, strengths and weaknesses, product launches, product range, and application dominance. However, the data points provided only focus on the companies’ activities related to the U.S. pharmacy benefit management market.
Prominent players in the market are expected to face tough competition from new entrants. Key players are targeting acquisitions of startup companies to maintain their dominance. The report
Reasons to Purchase this Report:
- Comprehensive market segmentation analysis incorporating qualitative and quantitative research, considering the impact of economic and policy factors.
- In-depth regional and country-level analysis, examining the demand and supply dynamics that influence market growth.
- Market size in USD million and volume in million units provided for each segment and sub-segment.
- Detailed competitive landscape, including market share of major players, recent projects, and strategies implemented over the past five years.
- Comprehensive company profiles encompassing product offerings, key financial information, recent developments, SWOT analysis, and employed strategies by major market players.
Key Market Players:
- CVS Health
- Cigna
- Optum, Inc.
- MedImpact
- Anthem
- Change Healthcare
- Prime Therapeutics LLC
- HUB International Limited.
- Elixir Rx Solutions LLC
Segment Covered in the Report:
By Business Model
- Standalone PBM
- Health Insurance Providers
By Service
- Specialty Pharmacy
- Retail Pharmacy
By End-user
- Commercial
- Federal
By Geography
- North America
- Europe
- Asia-Pacific
- Latin America
- Middle East and Africa
TABLE OF CONTENT
Chapter 1. Introduction
1.1. Research Objective
1.2. Scope of the Study
1.3. Definition
Chapter 2. Research Methodology (Premium Insights)
2.1. Research Approach
2.2. Data Sources
2.3. Assumptions & Limitations
Chapter 3. Executive Summary
3.1. Market Snapshot
Chapter 4. Market Variables and Scope
4.1. Introduction
4.2. Market Classification and Scope
4.3. Industry Value Chain Analysis
4.3.1. Raw Material Procurement Analysis
4.3.2. Sales and Distribution Channel Analysis
4.3.3. Downstream Buyer Analysis
Chapter 5. COVID 19 Impact on U.S. Pharmacy Benefit Management Market
5.1. COVID-19 Landscape: U.S. Pharmacy Benefit Management Industry Impact
5.2. COVID 19 – Impact Assessment for the Industry
5.3. COVID 19 Impact: Major Government Policy
5.4. Market Trends and Opportunities in the COVID-19 Landscape
Chapter 6. Market Dynamics Analysis and Trends
6.1. Market Dynamics
6.1.1. Market Drivers
6.1.2. Market Restraints
6.1.3. Market Opportunities
6.2. Porter’s Five Forces Analysis
6.2.1. Bargaining power of suppliers
6.2.2. Bargaining power of buyers
6.2.3. Threat of substitute
6.2.4. Threat of new entrants
6.2.5. Degree of competition
Chapter 7. Competitive Landscape
7.1.1. Company Market Share/Positioning Analysis
7.1.2. Key Strategies Adopted by Players
7.1.3. Vendor Landscape
7.1.3.1. List of Suppliers
7.1.3.2. List of Buyers
Chapter 8. U.S. Pharmacy Benefit Management Market, By Business Model
8.1. U.S. Pharmacy Benefit Management Market, by Business Model, 2023-2032
8.1.1 Standalone PBM
8.1.1.1. Market Revenue and Forecast (2020-2032)
8.1.2. Health Insurance Providers
8.1.2.1. Market Revenue and Forecast (2020-2032)
Chapter 9. U.S. Pharmacy Benefit Management Market, By Service
9.1. U.S. Pharmacy Benefit Management Market, by Service, 2023-2032
9.1.1. Specialty Pharmacy
9.1.1.1. Market Revenue and Forecast (2020-2032)
9.1.2. Retail Pharmacy
9.1.2.1. Market Revenue and Forecast (2020-2032)
Chapter 10. U.S. Pharmacy Benefit Management Market, By End-user
10.1. U.S. Pharmacy Benefit Management Market, by End-user, 2023-2032
10.1.1. Commercial
10.1.1.1. Market Revenue and Forecast (2020-2032)
10.1.2. Federal
10.1.2.1. Market Revenue and Forecast (2020-2032)
Chapter 11. U.S. Pharmacy Benefit Management Market, Estimate and Trends Forecast
11.1. U.S.
11.1.1. Market Revenue and Forecast, by Business Model (2020-2032)
11.1.2. Market Revenue and Forecast, by Service (2020-2032)
11.1.3. Market Revenue and Forecast, by End-user (2020-2032)
Chapter 12. Company Profiles
12.1. CVS Health
12.1.1. Company Overview
12.1.2. Product Offerings
12.1.3. Financial Performance
12.1.4. Recent Initiatives
12.2. Cigna
12.2.1. Company Overview
12.2.2. Product Offerings
12.2.3. Financial Performance
12.2.4. Recent Initiatives
12.3. Optum, Inc.
12.3.1. Company Overview
12.3.2. Product Offerings
12.3.3. Financial Performance
12.3.4. Recent Initiatives
12.4. MedImpact
12.4.1. Company Overview
12.4.2. Product Offerings
12.4.3. Financial Performance
12.4.4. Recent Initiatives
12.5. Anthem
12.5.1. Company Overview
12.5.2. Product Offerings
12.5.3. Financial Performance
12.5.4. Recent Initiatives
12.6. Change Healthcare
12.6.1. Company Overview
12.6.2. Product Offerings
12.6.3. Financial Performance
12.6.4. Recent Initiatives
12.7. Prime Therapeutics LLC
12.7.1. Company Overview
12.7.2. Product Offerings
12.7.3. Financial Performance
12.7.4. Recent Initiatives
12.8. HUB International Limited.
12.8.1. Company Overview
12.8.2. Product Offerings
12.8.3. Financial Performance
12.8.4. Recent Initiatives
12.9. Elixir Rx Solutions LLC
12.9.1. Company Overview
12.9.2. Product Offerings
12.9.3. Financial Performance
12.9.4. Recent Initiatives
12.10. Abbott
12.10.1. Company Overview
12.10.2. Product Offerings
12.10.3. Financial Performance
12.10.4. Recent Initiatives
Chapter 13. Research Methodology
13.1. Primary Research
13.2. Secondary Research
13.3. Assumptions
Chapter 14. Appendix
14.1. About Us
14.2. Glossary of Terms
Contact Us:
Mr. Alex
Sales Manager
Call: +1 9197 992 333
Email: sales@precedenceresearch.com
Web: https://www.precedenceresearch.com
Blog: https://www.expresswebwire.com/
Blog: https://www.uswebwire.com/
